Oh No! Tennis Elbow!

By Melissa Baudo Marchetti, PT, DPT, SCS, MTC
Is your elbow giving out on you when you play tennis? Do you feel pain whenever you grip your racket, type, text, write, carry something, or shake hands? You may be suffering from tennis elbow.
Tennis elbow, clinically referred to as Lateral Epicondylitis, plagues approximately 40-50% of all recreational racquet sport athletes at some point in their career with most cases occurring after age 30. Tennis elbow is a common overuse tendon injury that is caused by repetitive overload of the extensor tendons on the outside of the elbow resulting in pain, inflammation, weakness and degeneration (microtearing), making tennis and daily activities challenging, and at times impossible.
The primary symptoms include pain on the outside of the elbow and along the forearm, pain with gripping the racquet, and with wrist movements that occur with the forehand or backhand. Poor technique, ill-
Poor technique during the backhand stroke is a contributing factor in tennis elbow. If the elbow leads ahead of the stroke, more force is placed on the elbow as the racquet strikes the ball. Tennis players with a one-handed backhand are at higher risk for tennis elbow. The tennis serve also places high load on the elbow. If you are not using your legs efficiently and bending your knees as you serve, you will “pull through” your trunk to strike the ball, which places more force through the elbow and shoulder. Bending your knees during your serve allows your hips and trunk to rotate into optimal position to transfer the ground reaction forces into the legs and hips allowing you to “push through” your trunk generating optimal racket head and ball speed while minimizing the load on the shoulder and elbow. Racket head size, string tension and type, weight and grip size all contribute to tennis elbow and should be properly fit to the individual.
Initially, as the muscle and tendons are repetitively overloaded, local inflammation causes pain in your elbow and over time as the activity continues, the tendon and muscles weaken, and microtears and adhesions form. You may try resting for a week or two and taking some Advil, which may initially help decrease your pain, but even though the pain may be better, sensorimotor deficits, such as reaction time, speed, and muscle weakness persist even without you knowing. Then, you attempt to go back onto the court and the pain returns. Sound like you? Without proper management, pain will worsen, proper healing will not occur, and the tendon continues to degenerate, classifying the injury as Tendinopathy. Inflammation seems to play a role in the initiation of the injury, but not in the progression of the disease process, which is why anti-inflammatory medication and ice cease to manage your pain. The good news is that physical therapists have the tools to help restore your elbow range of motion and strength. For those of you who played way too long on a bad elbow may need more aggressive treatment interventions, but physical therapy is a good start.
Non-surgical treatment for tennis elbow should be considered first since it can heal the condition:
Rest. The first step toward recovery is to give your arm proper rest. This means that you will have to take a break from tennis for a few weeks. Your injury can worsen if you continue to play on your painful elbow.
Ice. The application of ice to the painful area of your elbow in the early phase of the injury can be helpful to minimize your symptoms. You can either use a bag of ice for approximately 20 minutes or an ice massage for 3-5 minutes directly over the painful area.
Equipment Check. Your equipment may be a contributing factor in your tennis elbow. So, consult with your tennis professional or coach to ensure proper fit of your racket, grip and strings.
Bracing & Taping. Using a counterforce brace or tape may be helpful in alleviating some of your symptoms.
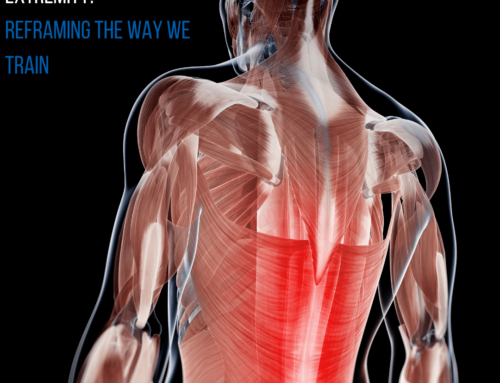
Physical Therapy. Restoring joint and soft tissue mobility, flexibility, strength, neuromuscular control, and movement patterns are the primary focus of physical therapy. PTs utilize an array of treatment techniques for the management of tennis elbow. Dry needling treats the rope-like “knots” within the forearm muscles. It may be uncomfortable, but it works! Manual therapy techniques are utilized to restore normal motion in the elbow joint and soft tissue as well as addressing restrictions in the adjacent shoulder, scapulae, and spine. Stretching to the forearm, elbow, shoulder, neck and back are implemented in the treatment of tennis elbow. Once your pain starts to decrease, eccentric training with bands, weights, suspension, and the flexbar are implemented to restore normal strength to the elbow, wrist and shoulder. Global strength and core training are also introduced once your pain begins to subside in order to get you ready to return to the court.
It is becoming more common for orthopedists to perform a diagnostic ultrasound during an office visit to identify the severity of your tennis elbow by looking for tears in the tendon. Corticosteroid injections have typically been utilized in the early stage of tennis elbow. However, many orthopedists are moving away from corticosteroids as some studies show poor long-term outcomes with the risk of re-injury and slow recovery times, and better long-term results with rest and physical therapy.
If you have failed conservative physical therapy treatment with little to no progress, and the tendon is damaged or torn, there are still options available to help you.
Platelet-rich Plasma (PRP) Injections. PRP is a biological blood-derived product from your own blood that is composed of platelets, white blood cells and growth factors that are injected into the tendon tear to stimulate the body’s natural healing response. The rehab process following PRP is long (no tennis for approximately 2-3 months), but the research thus far shows promising long-term outcomes.
Surgery. Minimally invasive surgery is available that aims to remove the damaged tissue so that new tendon can be laid down and proposes a quicker recovery with less time away from tennis. Consult your orthopedist to discuss your options.
Conclusion
Tennis elbow is a common tendon injury seen in recreational tennis players that is a result of repetitive overload. Tennis elbow is a preventable and often correctable injury. Ensure that you have been properly fitted with your equipment. If you are feeling pain in your elbow, consult your physical therapist and doctor as soon as possible in order to get an accurate diagnosis about the stage and severity of your injury and the integrity of the tendon. You may need to take some time off tennis to rehab your injury because continuing to play with pain can progressively worsen the injury sidelining you longer. Once your pain resolves and you are on the mend, gradually ramp up your tennis and return to the court. Play in moderation and continue your stretching and strengthening to prevent reoccurrence. It is not normal to have pain in your forearm or elbow during or after playing tennis so take advantage of the many treatment options and preventative strategies available so you can get back on the court.
Dr. Baudo Marchetti is a Board Certified Sports Clinical Specialist at One on One Physical Therapy, a multidisciplinary private practice in Atlanta. For nearly five years she was a full-time sports physiotherapist for the WTA Tour and is a tennis medicine expert. She teaches a Sports Physical Therapy course and assists in teaching orthopedics within the Division of Physical Therapy at Emory University. Learn more by visiting www.onetherapy.com. Special thanks to Aylin Seyalioglu, PT for her contribution to this article.