Bending without breaking: Hypermobility disorders and physical therapy
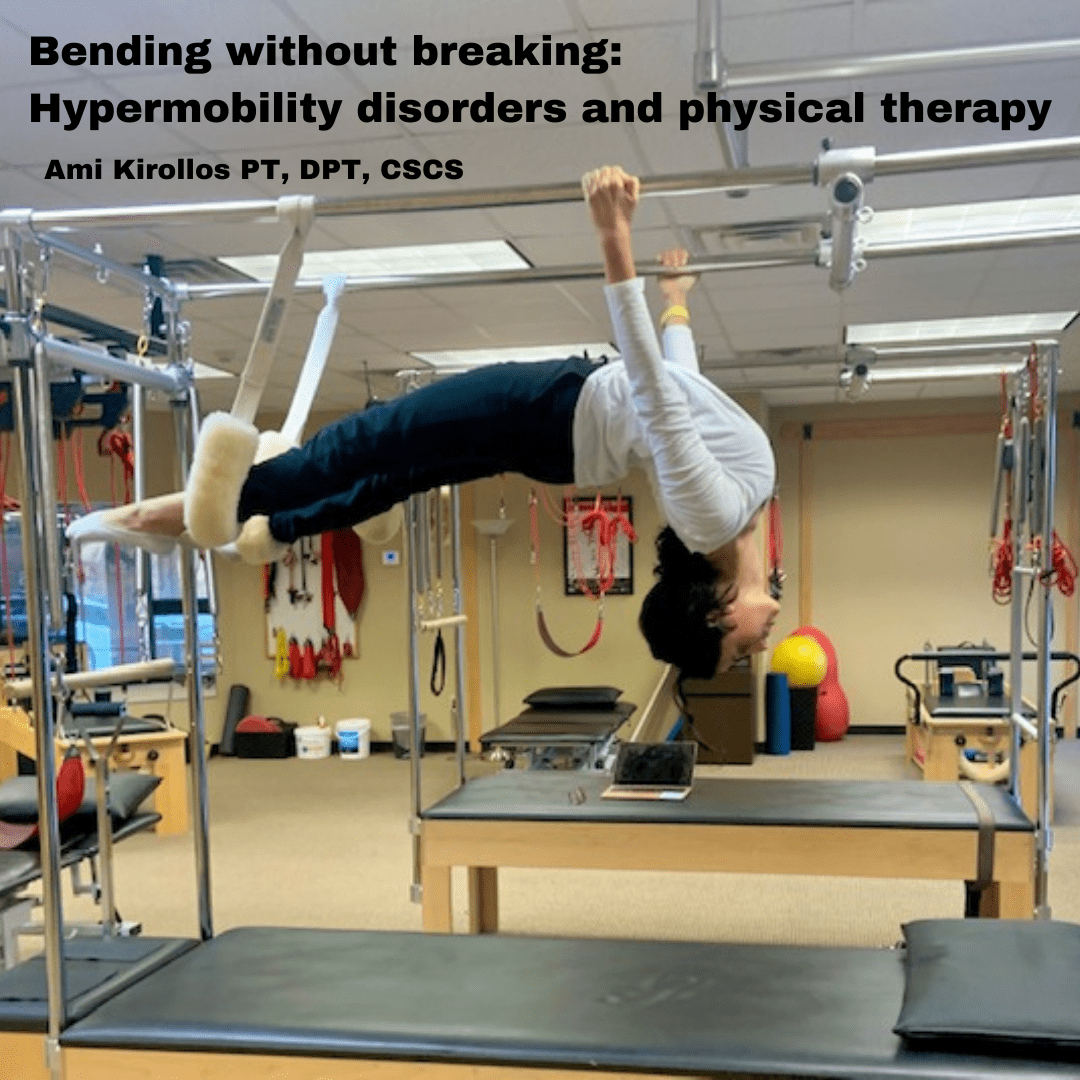
“Hypermobility,” is a term we like to throw around in all types of ways. For many people, it means casually bringing your leg over your head in yoga class or twisting your body into a pretzel-like Cirque Du Soleil performer, but for others, it means chronic pain, frequent injuries, and symptoms that many medical providers will shrug off as “being bendy.”
There is a fine line when “flexible” can be more than just limber joints and muscles and may be part of a more complex condition.
Drum roll, please… Enter “Ehlers Danlos Syndrome” and “Hypermobility Spectrum Disorders.”
Ehlers Danlos Syndrome (EDS):
Is a hereditary disorder of our bodies’ connective tissues. With EDS collagen (the substance that makes up connective tissues) is abnormal. This being the underlying concern of EDS as it can cause increased laxity in not only the joints and muscles but in rare subsets of the condition can also cause excessive laxity in our vessels (veins, arteries) and organs. Although EDS is relatively rare, because of its varied symptoms and presentation it often goes undiagnosed, and thus treated improperly.
Oftentimes EDS’s presentation has 3 hallmark symptoms of dysautonomia, hypermobile joints, and skin abnormalities, however can vary from case to case.
Hypermobility Spectrum Disorders (HSD’s:)
More common than EDS, are HSD’s. This is a group of hypermobility disorders that are often diagnosed after EDS has been ruled out by a medical provider. These disorder’s symptoms can range from being asymptomatic to being very symptomatic, with major impacts on an individual’s life. Similar to EDS these disorders present with increased ranges of motion at many or just certain joints in the body, but unlike EDS do not usually present with as much of a collagen abnormality, and symptoms are often more musculoskeletally based.
What hypermobility may look like:
- Decreased sense of joint position in space: At times those with hypermobile joints may lack awareness of where the heck the joint is in space, leading to increased injury as we allow our bodies to land, step, or jump with decreased control.
- Frequent injury or chronic pain: this may manifest in a number of ways. Increased range of motion at joints leading to increased dislocation or subluxation injuries, increased joint pain, muscle tightness around hypermobile joints, nerve pain, and increased sensitivity and inflammatory response throughout the body.
- Skin issues: some individuals with HSD or EDS will have “stretchy” skin, poor or delayed healing of scars, and may easily bruise/tear their skin.
- Pelvic floor: Just like other muscle groups, increased mobility, and laxity of pelvic floor muscles may be present with hypermobility as well. Some individuals will be more likely to experience conditions such as prolapse, incontinence, and pelvic pain because of this. Confused? Check out our blog on Hypermobility and Pelvic Floor!
- GI symptoms: Symptoms such as constipation, slowed digestion, and irritable bowel syndrome has been correlated with some hypermobility disorders.
- Dysautonomia: a blanket term for a group of disorders that impact our autonomic nervous system which controls things like breathing, heart rate, and blood pressure (kind of important.) Often those with EDS have trouble regulating this system at times and may experience symptoms like lightheadedness, nausea, sweating, fatigue, tachycardia (increased heart rate,)palpitations, or headaches from simple triggers such as standing up straight.
- Increased likelihood of anxiety disorders: some research suggests those with hypermobility syndromes or EDS are more prone to certain mood disorders and sleep disturbances.
A brief pause for a quick “Myth Buster:”
Individuals with HSD and EDS always present with a lot of flexibility: FALSE. Although your joints may be very mobile, sometimes this causes muscles and other soft tissues around the joints to “clench” or become tight and restricted, decreasing motion.
How is HSD and EDS “Diagnosed:”
If you suspect you may have an underlying hypermobility condition the first step is to inform your medical provider. If you wish to pursue an official diagnosis, referral to a specialist such as a Rheumatologist or Genetic specialist for the appropriate testing may be merited.
From there, an interprofessional approach is taken to manage symptoms. This team approach may include physical therapy, pain management specialist, behavioral therapies, personal trainer, or massage therapist.
Additionally, you can screen yourself at home with the “Beighton Score” test. This is a movement screening that may give you an idea of whether you may have some hypermobility. A score of 5 out of 9 points for adults is considered “positive.”
*Disclaimer, this NOT diagnostic, but informational*
Check out this video of the brief screening:

Standing with knees locked out. Does your lower leg extends more than 10 degrees forward? one point on each side.

Elbows stretch out to the side fully extending. Do you have more than 10 degrees bend with elbow backward? one point on each side.
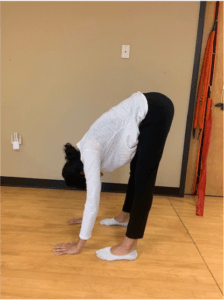
Can you bend forward and place palms flat on the floor without bending your knees? One point.

With arms straight, Does the thumb touch the forearm? One point on each side.

Does your 5th finger when placed palm down extend past 90 degrees when lifted? One point on each side.
Physical Therapy for Hypermobility:
For individuals struggling with hypermobility disorders of any kind, physical therapy is an effective and recommended way to manage and treat symptoms.
Signs and symptoms Physical Therapy can help with:
- Chronic pain symptoms: Techniques such as Trigger Dry needling, soft tissue manipulation, myofascial release, and pain science education have been proven to help symptoms of chronic pain that may be associated with HSD or EDS.
- Decreased motor control and stability: to address hypermobility PT will focus on education and retraining the body to promote stability at hypermobile joints, awareness of joint position, and ensure proper alignment and execution of daily tasks, exercises, and posture to prevent further exacerbation of symptoms of hypermobility and prevent injury.
- Pelvic floor dysfunction: Working with a pelvic floor specialist can promote strength and stability in the pelvic floor muscles allowing them to support abdominal organs and relieve symptoms caused by diagnoses such as prolapse, pelvic pain, or incontinence.
- Graded exercise progression: Exercising with an underlying hypermobility disorder is a tricky game. It requires a specific gradual exposure and build-up to avoid injury or flare-up of pain symptoms. It may require a guided and individualized approach. See below for some tips on exercise progression for hypermobility.
Starting an Exercise program for individuals with HDS or EDS:
- “Start low, and Slow”: as Dr. Lussek researcher and Physical therapist at Clarkson University suggest. it may take 4-6 weeks to progress past simple non-weighted stabilization exercises, and that’s okay!
- Focus on stability: Those joints need stability! Try to focus on exercises that promote support and stability for your body, rather than an overemphasis on prolonged stretches. For example strength training (gradually increasing weight,) pilates, or Gyrotonic
- Time and intensity: increase time no more than 20% per week, working up to 30 minutes per day. Once this is achieved without increased pain or symptoms, try increasing other variables like weight or speed.
- Listen to your body and reassess: Overdid it? Don’t despair, recognize where your body is in its journey, and respect that. The hypermobile body requires patience, but is one hundred percent capable of achieving gains in strength and stability, just like anyone else! Take a step back, and work your way up!
Interested in learning more about physical therapy for hypermobility disorders?
Here are some resources:
- The Ehlers-Danlos Society: a plethora of resources and information for those with EDS or HSD: https://www.ehlers-danlos.com/assessing-joint-hypermobility/
- Linda Bluestein, “Hypermobility MD”: For my DANCERS! Check out her website, blog, and book “Disjointed”! All are great resources for individuals with hypermobility, most especially those in the dance community: https://www.hypermobilitymd.com
Want even more? Contact us at One on One Physical Therapy to schedule an appointment today!
Disclaimer: many symptoms of EDS and HSD are very common in the general public, making it easy to self-diagnose yourself with one (I see you my “WebMD” people.) So if some of these symptoms seem familiar, do not panic! Feel free to have a conversation with your healthcare provider (or PT.)
Works Cited:
Bluestein, Linda. (n.d.). Hypermobility Specialist: Medical Services for Dancers: United States. Hypermobility MD. https://www.hypermobilitymd.com/.
Russek, L. (n.d.). Ehlers-Danlos/Hypermobility Spectrum Disorder.
What are hypermobility spectrum disorders? The Ehlers Danlos Society. (2021, May 4). https://www.ehlers-danlos.com/what-is-hsd/.