Bladder Health Month: The Truth Behind Voiding Dysfunction
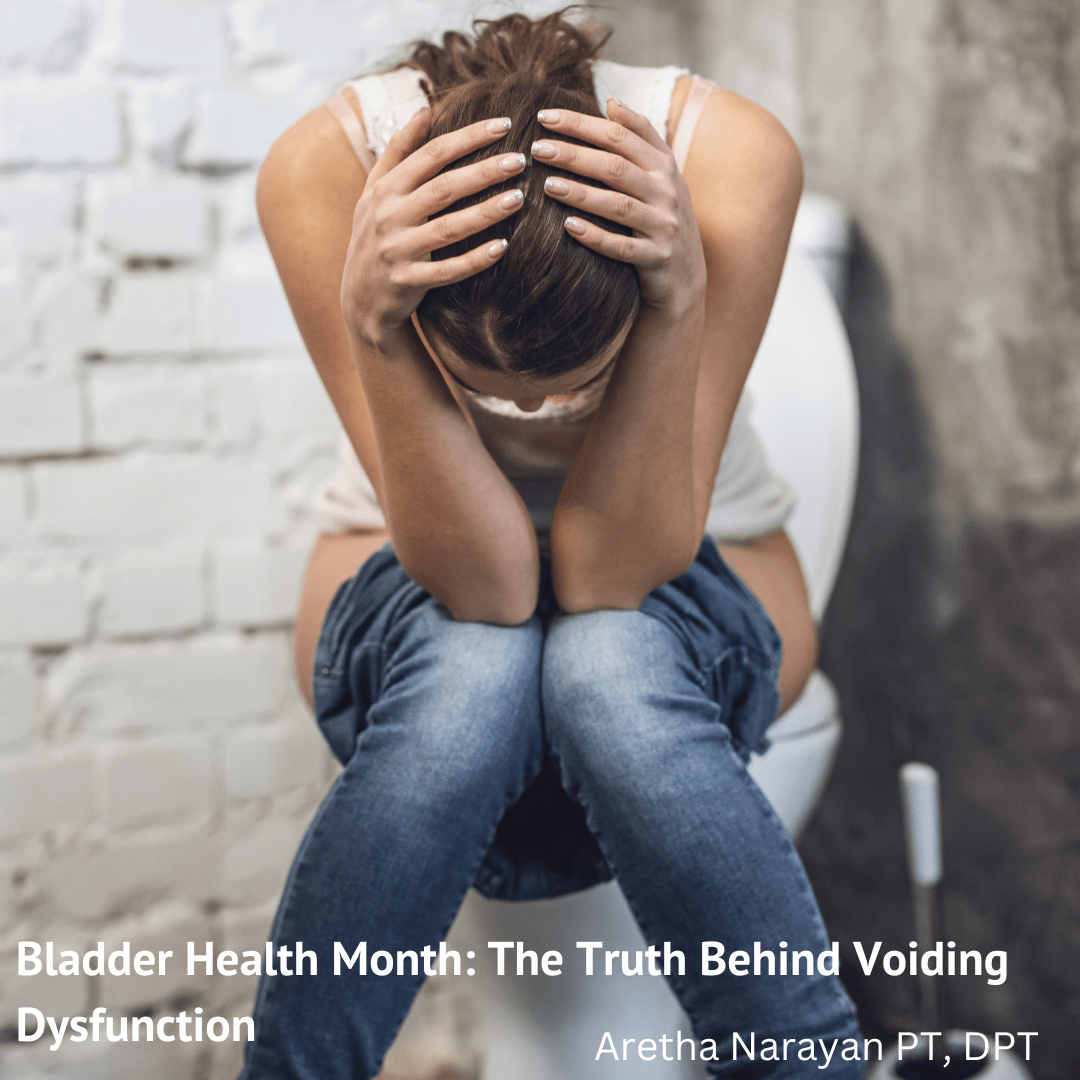
Bladder Health Awareness: How Physical Therapy Can Help
November isn’t just for turkey dinners and football games—it’s also Bladder Health Month! It’s the perfect time to raise awareness about bladder health and common urinary issues like voiding dysfunction that many people face but rarely talk about.
Do You Struggle with Urination?
- Do you find yourself sitting on the toilet, starting and stopping mid-stream?
- Are you making frequent trips to the bathroom, feeling like you “gotta go” every 30 minutes?
If you’re nodding yes, you’re not alone! These could be signs of bladder dysfunction, or voiding dysfunction, and understanding the root causes can help you regain control over your bladder and improve your daily life.
See Also: Gotta Go!
What is Voiding Dysfunction?
Voiding dysfunction refers to difficulties with starting, continuing, or fully emptying your bladder when you urinate. It includes issues like trouble initiating a stream, hesitancy (starting and stopping during urination), and retaining urine. These problems can significantly disrupt your routine and impact your quality of life.
The good news? You don’t have to suffer in silence. Voiding dysfunction is more common than many realize, and there are effective treatments available, especially through pelvic health physical therapy.
Common Causes of Bladder Dysfunction
Several factors can contribute to bladder dysfunction. Let’s take a closer look at some of the most common causes:
1. Overactivity of the Pelvic Floor Muscles
Your pelvic floor muscles play a crucial role in controlling urination. These muscles form the base of your core and need to contract and relax in coordination with your bladder.
- When your pelvic floor contracts, it signals your brain to relax the bladder muscles and stop the flow of urine.
- If the pelvic floor is overly tight and unable to relax properly, it can interfere with the bladder’s ability to empty, causing difficulties with starting or maintaining a stream.
This overactivity often leads to increased pressure on the urethra, making urination more difficult and uncomfortable.
2. Stress and Urination
Stress affects nearly every aspect of our health, and bladder function is no exception. When we’re stressed, it can become harder to relax our pelvic floor muscles, leading to problems with initiating urination or causing a stop-start pattern while peeing.
Relaxation techniques, such as diaphragmatic breathing, mindfulness, and meditation, can help reduce this tension and improve bladder control.
3. Learned Voiding Dysfunction
Over time, many of us develop unhealthy voiding habits without even realizing it:
- Maybe you squat instead of sitting in public restrooms.
- Or you’ve been stopping and starting your stream when someone walks into the restroom.
- Have you ever done “just in case” peeing before leaving the house?
These habits may seem harmless, but they can interfere with the normal function of the bladder-pelvic floor-brain relationship, leading to dysfunctional urination patterns.
4. Pelvic Adhesions
Scar tissue, or adhesions, can form after surgeries, infections, endometriosis, or other injuries affecting the pelvic region. These adhesions can disrupt the function of nearby organs, including the bladder, leading to symptoms like pain, bowel obstruction, or bladder dysfunction.
How Can Pelvic Health Physical Therapy Help?
If you recognize any of these symptoms in yourself, it might be time to consider pelvic health physical therapy. A pelvic health PT specializes in treating pelvic floor dysfunction and can help you regain control of your bladder through targeted treatments, including:
- Bladder retraining: Gradually teaching your bladder to hold urine for longer periods.
- Pelvic floor relaxation exercises: Helping your pelvic floor muscles learn how to properly relax.
- Manual therapy: Techniques to release tight muscles and improve mobility.
- Internal self-massage: Helping to reduce tension in the pelvic floor.
- Dilator therapy: For those with pelvic adhesions or tightness, dilators can help restore function.
Taking Control of Your Bladder Health
Bladder dysfunction can be frustrating, but there’s no need to let it control your life. A pelvic health physical therapist can work with you to develop a personalized treatment plan that addresses your specific needs, helping you regain confidence and improve your quality of life.
By understanding the causes of your symptoms and working with a skilled PT, you can get back to living your best life—without constantly worrying about finding the nearest bathroom.
If any of this sounds familiar, reach out to a pelvic health PT today!