The Nocebo Effect: How Your MRI Report Can Hurt You

MRI finding L5 disc herniation
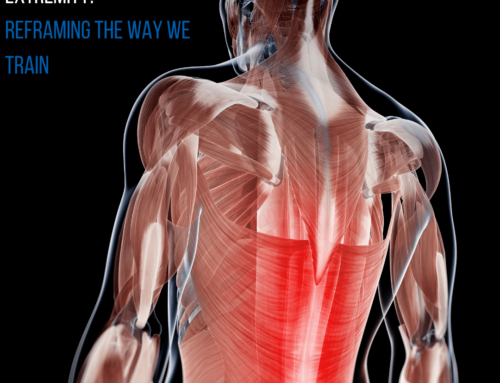
Ever been diagnosed with a tendon tear, disc bulge or degenerative disease of a joint based on an MRI report? Has a physician determined that this was causing your pain? If so, while the physician was correct as far as finding a variance in your body’s tissue, they may be incorrect in determining that this finding was the primary cause of the pain. Recent research indicates that many people without pain actually have findings on an MRI such as a herniated disc, rotator cuff tear, or meniscal tear. Research also shows that patients with pain who present with these same findings are getting better without surgery, and the MRI findings are not changing after they do so.
All MRI findings should be correlated with a thorough clinical assessment. There are times where the MRI findings are contributing to pain and/or may pose a serious threat where medical intervention or surgery may be warranted. However, in most cases, conservative physical therapy treatment may be all that is needed for pain reduction and to restore functional movement.
NOCEBO EFFECT
“It ain’t what you don’t know that gets you into trouble.
It’s what you know for sure that just ain’t so.” – Mark Twain
Physicians and Physical Therapists (PT’s) are changing the way they educate patients regarding musculoskeletal diagnostic findings. The informed clinician knows that these findings may not be related to the actual pain. They also know that telling a person that a body part is “damaged” and is causing their pain may very well make the problem worse. This is called the “nocebo effect”. The “nocebo effect” is the opposite of the more commonly understood “placebo effect”. Studies show that merely suggesting that an experimental treatment will increase muscle pain will cause people to feel pain at lower levels of stimuli than prior to being told this.
The history of treating pain has been based on inaccurate knowledge that has mis-shaped our society’s understanding of pain. This has created deceiving experiences for people that have caused inaccurate beliefs and thoughts that the pain is being caused by irreversible damage, and that surgery is the only way to reduce the pain. The medical community now understands, based on functional MRI studies of the brain, that fear of damage, negative thoughts, frustration and anxiety will considerably amplify, prolong and, in some cases, cause pain.
A COMMON WRINKLE
Disc bulges or herniations are among the most common findings on MRIs that are often erroneously associated with low back pain and sciatica (pain down the leg). A study completed in 2015 reviewed MRI results of 1211 pain-free people. They found that 87.6% of people over 30 years old had disc bulges, but had no pain. 75% of people in their 20’s also had the same findings. It appears that disc herniations are as common as skin wrinkles and a normal part of the aging process, but are not highly correlated with pain. A very common cause to low back pain and sciatica are muscle trigger points in the low back and hip. These trigger points can be effectively treated by manual therapy, foam rolling, massage, and trigger point dry needling. Trigger points are often the result of muscular or postural imbalances that can be identified by your PT and corrected with specific exercises.
While persistent pain may be caused by tissue damage found on MRI, often it is not. Ensure that your care is thorough by having a skilled Physical Therapist assess and treat muscular, joint and nerve related pain as early as possible. Less threatening and easier to resolve problems can often be identified and treated quickly and effectively. If more concerning problems exist that require diagnostic images and further medical intervention, the PT can get you directed to an appropriate physician. Persistent pain is almost always multifactorial. Our thoughts, beliefs, fears and anxieties play a significant role. By decreasing undue nocebo effects associated with pain, one can make great strides in regaining lost balances in body and mind.
Lance Cross, PT, MPT, OCS, CMTPT is a Board Certified Orthopaedic Physical Therapist at One on One Physical Therapy. His particular background in the pain sciences includes clinical treatment of chronic pain patients, lecturing and involvement in clinical trials on the subject. He is a Certified Sports Metrics Trainer and has particular involvement in knee injury prevention program development. Lance implements various manual therapy techniques, dry needling, Redcord & The Neurac Method and Pilates for Rehabilitation into his comprehensive treatment approach. He enjoys cycling in all disciplines and is frequently found cyclocross racing or mountain-biking with his wife and friends in the mountains. Lance offers free consultations at One on One Physical Therapy. Learn more by visiting www.onetherapy.com or email lance@onetherapy.com.