Do You Know Your Vulva?
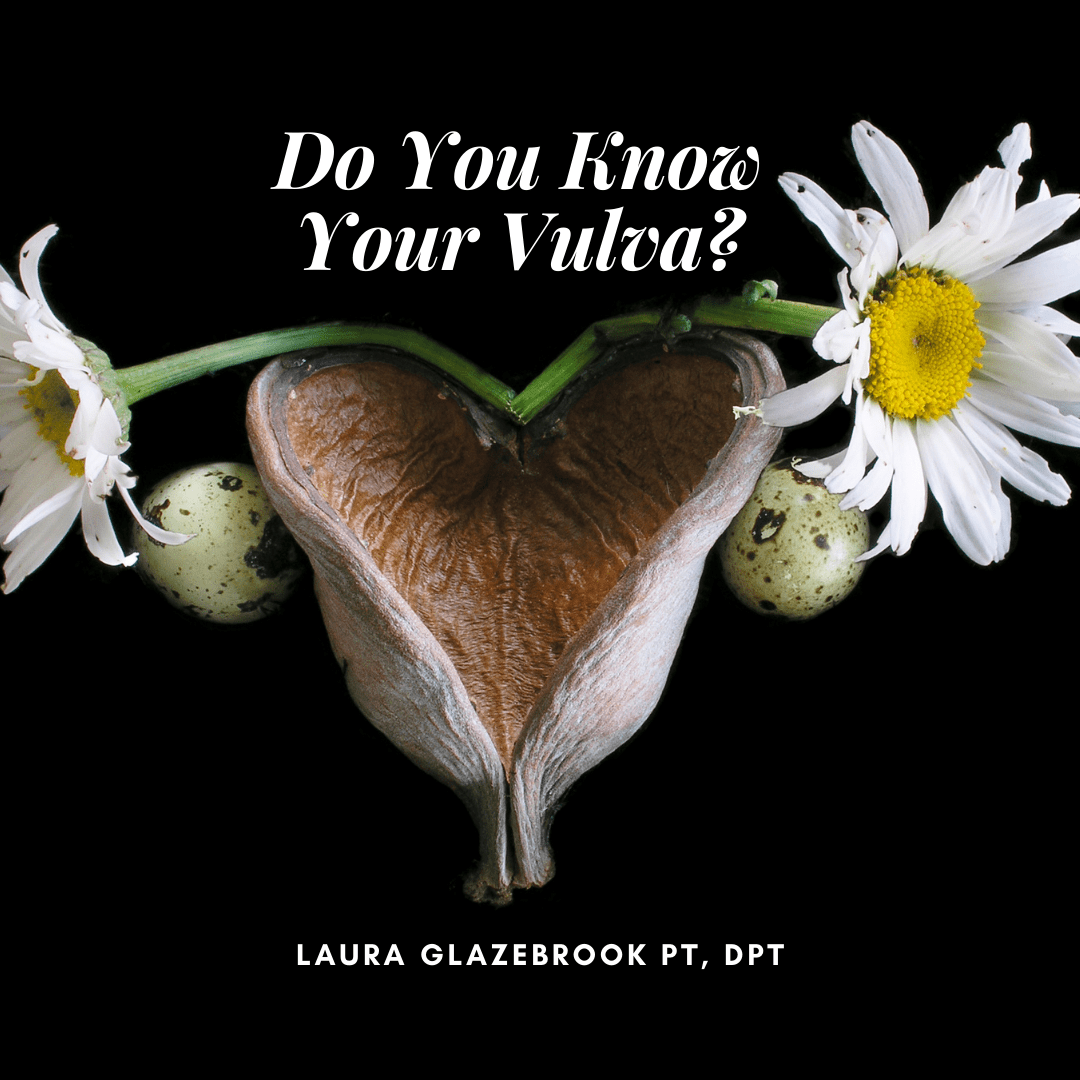
Do you Know your Vulva? Anatomical names are important!
This post is specifically for the ladies, or anyone with a vulva… which is different from a vagina! The vulva is the name of the outer portion of genitalia in which the vagina sits. According to this article from the New York Post, up to 46% of American women surveyed couldn’t point out their cervix, and 57% couldn’t identify the uterus. Only one in 10 were able to correctly complete a female reproductive diagram. So, without further ado, here’s an illustration of our anatomy “down below”…
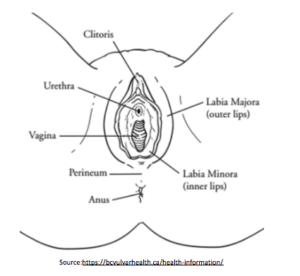
source: https://bcvulvarhealth.ca/health-information/
The clitoris is quite a bit more expansive than the picture makes it look, with a healthy blood supply and thousands of nerve endings responsible for orgasm. What is shown in the picture is actually the clitoral hood. When aroused, the clitoris engorges with blood similar to the penis.
The urethra is the hole where the urine leaves our body.
The vagina, or introitus, is connected to the uterus. This is where a penis or toy would enter for penetrative sex, also where a baby would exit during childbirth.
The two sets of labia (majora and minora) are the lips which protect the urethra and vagina.
The anus lays outside of the labia, separated by a band of tissue called the perineum.
Every vulva looks different, and that is okay! Sometimes the inner labia extend past the outer and sometimes not, they aren’t always symmetrical, and sometimes the appearance changes after childbirth. Everyone would benefit from exploring their vulva. Being aware of its appearance and what “normal” looks like is crucial to be able to identify when there is an issue, like skin changes or vulvar cancer. At the very least, understanding one’s own genital anatomy can enhance sexual experience, either alone or with a partner.
Fun Anatomical Facts:
- Everyone is formed with the same muscles, and whether they will develop into a penis or a vagina is determined by our DNA.
- The pelvic floor muscles are some of the first to form.
- Much like the mouth and the gut, the vagina has its own microbiome, a complex ecosystem of microorganisms that colonize the vagina. It is dynamic, changing during the menstrual cycle, with pregnancy, and after menopause. Using soaps or feminine hygiene products may disrupt the delicate balance and lead to infections.
Common Conditions of the Vulva and Vagina Include:
Vulvodynia and Vestibulodynia→ hypersensitivity in the skin of the vulva or vagina causing irritation, sensation of itching or pain
Vaginismus→ involuntary contraction or overactivity of the pelvic floor muscles, sometimes referred to as pelvic floor spasms. Overactive pelvic floor muscles can cause discomfort or pain during sex or using a tampon, as well as difficulty having a bowel movement. This can be congenital (starting from birth) or due to other factors such as our alignment, muscle imbalances or history of trauma.
Lichen sclerosus, vulvar lichen planus→ skin changes including whitening and hardening of the vulvar skin, can lead to irritation and pain
Candidiasis/ Yeast Infection→ itching, soreness or burning in the vagina or vulva, sometimes following sex. This is typically accompanied by a strong odor and discharge, but not always.
Bacterial Vaginosis→ overgrowth of one type of bacteria which can be accompanied by itching or burning during urination, as well as discharge and odor.
Unfortunately, due to the complex nature of vulvar and vaginal health, sometimes the symptoms can be misleading. As you can see from above, some symptoms overlap between different conditions, such as burning while voiding the bladder or more urgency to go to the bathroom. Many patients will feel they have a urinary tract infection when they experience these symptoms but aren’t sure where to go next when they test negative. There is a wealth of information in the form of handouts on the ISSVD website to learn more.
Your Interdisciplinary Healthcare Team
As with any condition, you may be best served by a team of specialized healthcare providers. It is important to know that vulvar health is complex. While there is no one expert or specialist, many providers can help get you some relief. Try not to get frustrated with any one provider for not having all the answers! Giving a thorough background will assist your provider in making an accurate treatment plan.
This team may include:
- Pelvic Floor Physical Therapist
- Vulvar Dermatologist
- Neurologist
- Gynecologist, Urologist or Urogynecologist
The Role of Pelvic Floor Physical Therapists in Restoring Vulvovaginal Health
A Pelvic Floor Physical Therapist has specialized training to assess the vulva and the pelvic floor muscles, as well as plenty of tools to teach you about how to obtain and maintain optimal health. We also know which providers would be best suited to help address any issues, get testing or medications as needed.
If you or someone you know is experiencing these issues, contact our clinic and schedule an evaluation today!
Resources
Search for a vulvar dermatologist
International Society of the Study of Vulvovaginal Disorders — Resource Library