Male Pelvic Health: Pudendal Neuralgia
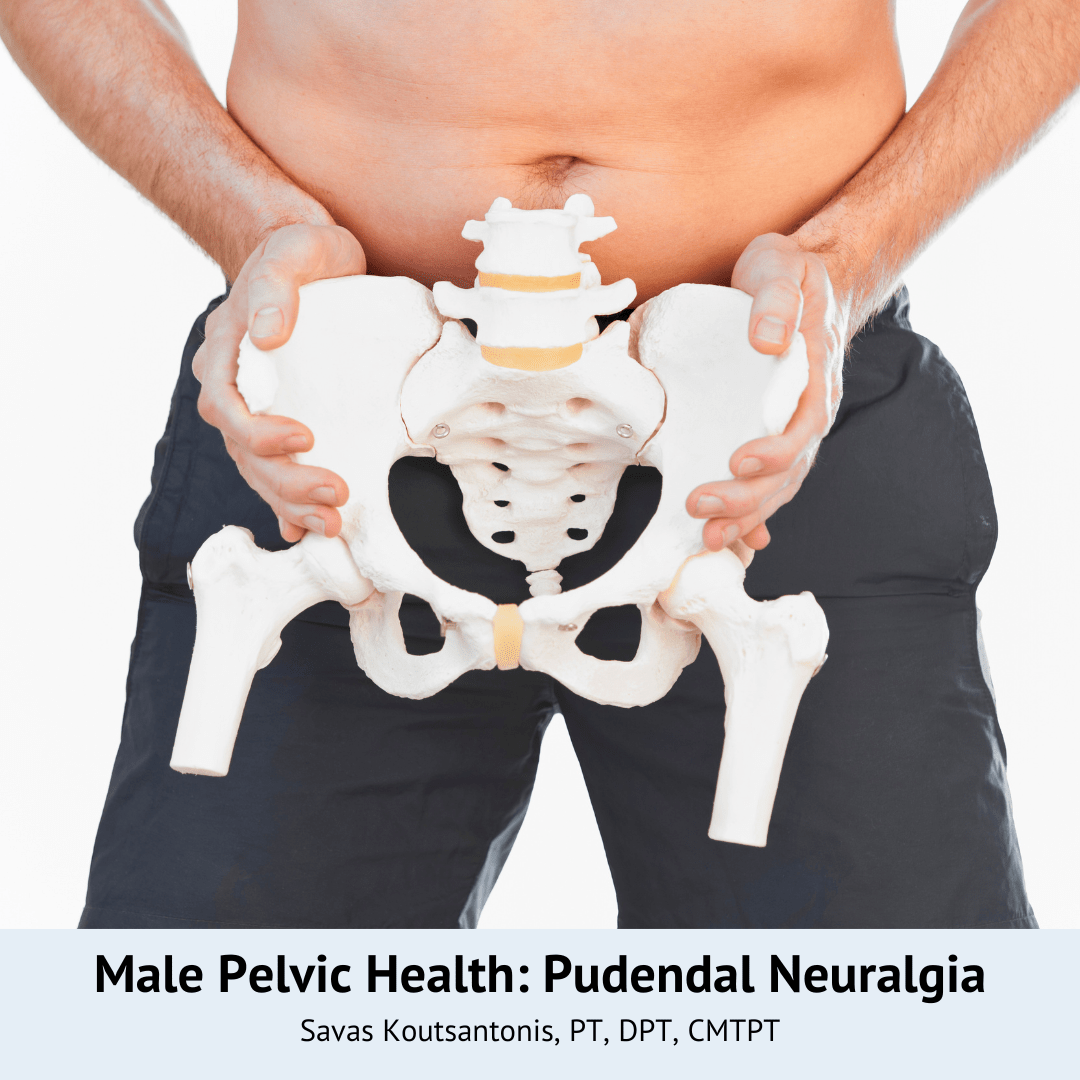
Pudendal Neuralgia Men: Causes, Symptoms, and Treatments
Pudendal Neuralgia in Men is a condition that causes severe and persistent pelvic pain due to irritation, compression, or damage to the pudendal nerve. This nerve is a critical structure in the pelvis, responsible for sensory and motor control of the pelvic floor muscles, the external anal sphincter, and parts of the genital area, including the glans penis in men. When the pudendal nerve is compromised, it can lead to chronic pain, sexual dysfunction, and various forms of pelvic dysfunction. Pudendal neuralgia is often underdiagnosed, particularly in male patients, many of whom delay seeking treatment.
Pudendal neuropathy, a related condition, is rare and often underreported in the general population. It can be caused by factors such as pelvic trauma, prolonged sitting, and physical activities that may cause nerve compression or stretch.
This article will provide an in-depth understanding of pudendal neuralgia in men, covering the pudendal nerve‘s anatomy, the causes of pudendal nerve entrapment, common pudendal neuralgia symptoms, and how pudendal neuralgia treatment, including physical therapy, can provide relief.
What is Pudendal Neuralgia?
Pudendal neuralgia refers to the pain and dysfunction caused by irritation or compression of the pudendal nerve, a nerve that runs through the pelvis. In men, this nerve plays a vital role in controlling the pelvic floor muscles, the external genitalia, and bowel and bladder functions. The pudendal nerve is divided into three main pudendal nerve branches:
- Inferior rectal nerve: Controls the external anal sphincter and provides sensory input to the anal canal.
- Perineal branch: Innervates the pelvic floor muscles, the urethral sphincter, and provides sensory information to the perineum and scrotum.
- Dorsal nerve: Provides sensation to the glans penis.
When the pudendal nerve is compressed or irritated, it can cause nerve pain in any of these areas, leading to pudendal nerve pain, sexual dysfunction, and other symptoms. In men, pudendal neuralgia can result in penile pain, scrotal pain, and perineal pain, which may worsen with prolonged sitting or certain activities like cycling or heavy lifting. Pudendal neuropathy, often underreported, can arise from causes such as pelvic trauma, prolonged sitting, and physical activities that may cause nerve compression or stretch.
Clinically Relevant Anatomy
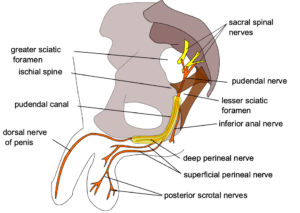
Understanding the anatomy of the pudendal nerve is crucial for comprehending how pudendal neuralgia develops and affects the body. The pudendal nerve originates from the sacral plexus, specifically the S2-S4 nerve roots. It travels through the pelvis, passing through the greater sciatic foramen, around the ischial spine, and into the lesser sciatic foramen. This intricate path makes the pudendal nerve susceptible to entrapment and irritation at several points.
The pudendal nerve has three primary branches, each serving distinct functions:
- Inferior Rectal Nerve: This branch innervates the external anal sphincter and provides sensory input to the anal canal. Dysfunction in this branch can lead to rectal pain and issues with bowel control.
- Perineal Branch: Responsible for innervating the pelvic floor muscles and the urethral sphincter, this branch also provides sensory information to the perineum and scrotum. Problems here can result in perineal pain, urinary dysfunction, and discomfort in the scrotal area.
- Dorsal Nerve of the Penis: This branch supplies sensation to the glans penis. When affected, it can cause penile pain and contribute to erectile dysfunction.
The pudendal nerve’s complex route and its critical role in sensory and motor functions of the pelvic region underscore why any irritation or compression can lead to significant discomfort and dysfunction. Understanding this anatomy helps in diagnosing pudendal neuralgia and tailoring effective treatment strategies.
Causes of Pudendal Neuralgia in Men
Several factors can contribute to pudendal nerve entrapment and pudendal neuralgia in men. These include:
- Pelvic floor dysfunction: Tight or hypertonic pelvic floor muscles can compress the pudendal nerve, leading to nerve pain and pelvic discomfort.
- Direct trauma: Injuries to the pelvic region from falls, accidents, or even pelvic surgery can damage or irritate the pudendal nerve.
- Prolonged sitting: Activities that involve sitting for extended periods, such as biking or desk jobs, can place prolonged pressure on the pudendal nerve, leading to chronic pain.
- Pelvic surgery: Surgeries such as hernia repairs or prostate surgery may inadvertently affect the pudendal nerve, leading to post-surgical complications like pudendal neuralgia or pudendal nerve damage.
- Sports injuries: High-impact sports or exercises that involve bearing down, such as weightlifting, can compress the pudendal nerve and contribute to nerve entrapment.
- Sacroiliac joint dysfunction: Misalignment of the sacroiliac joints, located in the pelvis, can indirectly impact the pudendal nerve, leading to chronic pelvic pain.
Pudendal neuropathy can result from similar factors, such as pelvic trauma, prolonged sitting, and physical activities that may cause nerve compression or stretch.
Symptoms of Pudendal Neuralgia in Men
The symptoms of pudendal neuralgia vary depending on which pudendal nerve branches are affected. Common symptoms in men include:
- Penile pain or genital pain: Often described as burning or sharp pain that worsens with sitting or sexual activity.
- Scrotal pain: A deep, aching sensation in the scrotum that may radiate to the perineum or thighs.
- Rectal pain: Discomfort in the anal canal or a sensation of a foreign object in the rectum, especially when sitting.
- Urinary dysfunction: Difficulty urinating, urinary urgency, or painful urination can occur when the pudendal nerve is involved.
- Erectile dysfunction: Damage to the dorsal nerve of the penis can lead to erectile dysfunction and pain during or after sexual activity.
- Pelvic pain: A general sense of pelvic pain or pressure, which may radiate to the lower back, buttocks, or thighs.
- Other symptoms: Flare-ups may cause sweating, increased heart rate, anxiety, and other autonomic responses to severe pain.
Diagnosis of Pudendal Neuralgia
Diagnosing pudendal neuralgia can be challenging as the condition is often underrecognized and overlaps with other pelvic pain syndromes. A physical examination by a specialist is crucial in determining pudendal nerve involvement. Diagnostic approaches include:
- Physical exam: A pelvic floor physical therapist or physician will assess the pelvic area, including the pelvic floor muscles, joints, and ligaments, to identify signs of pudendal nerve entrapment.
- MRI: This imaging technique can help rule out other causes of pelvic pain and detect abnormalities in the sacrotuberous ligaments, sacrospinous ligaments, or the pudendal canal.
- Pudendal nerve block: A pudendal nerve block involves injecting a local anesthetic into the pudendal nerve to provide temporary relief. If the block alleviates pain, it helps confirm pudendal nerve involvement.
- Electromyography (EMG): This test measures the electrical activity of muscles and nerves to identify nerve damage or dysfunction in the pelvic floor.
- Quantitative sensory testing: This diagnostic tool assesses nerve function by measuring responses to temperature, vibration, and pain stimuli, helping to identify neuropathic pain.
Pudendal Neuralgia Treatment for Men
Treatment for pudendal neuralgia often requires a multidisciplinary approach, focusing on pain relief, restoring function, and addressing the underlying causes of pudendal nerve pain. Common pudendal neuralgia treatments include:
1. Pelvic Floor Physical Therapy
Pelvic floor physical therapy is a cornerstone of pudendal neuralgia treatment. A specialized physical therapist will perform manual techniques to release tension in the pelvic floor muscles, including the obturator internus muscles, which can compress the pudendal nerve. Treatment may also involve:
- Trigger point release: Targeting areas of tight muscle tissue to reduce pain and nerve compression.
- Joint mobilization: Restoring mobility to the sacroiliac joints and hips to relieve pressure on the pudendal nerve.
- Biofeedback and neuromuscular re-education: Helping patients gain control over the pelvic floor muscles to improve bladder, bowel, and sexual function.
2. Nerve Blocks
Pudendal nerve blocks can provide temporary relief from pudendal nerve pain by reducing inflammation around the nerve. Nerve blocks may be repeated periodically to help manage pain, and they can also assist in confirming the diagnosis.
3. Medications
Medications for pudendal neuralgia may include:
- Muscle relaxants: To relieve tightness in the pelvic floor muscles and reduce nerve compression.
- Neuropathic pain medications: Such as gabapentin or pregabalin, which can help reduce nerve pain by stabilizing overactive pain signals.
- Anti-inflammatory medications: To reduce swelling and irritation around the pudendal nerve.
4. Surgical Decompression
For cases of chronic pudendal neuralgia where conservative treatments have not provided relief, pudendal nerve decompression surgery may be considered. This decompression surgery aims to release the pudendal nerve from areas of entrapment, such as the ischial spine or sacrotuberous ligaments.
5. Spinal Cord Stimulation
In rare and severe cases, spinal cord stimulation may be used to disrupt pain signals sent from the pudendal nerve to the brain. This technique involves implanting a device that sends electrical pulses to the spinal cord, helping to mask the pain.
6. Alternative Therapies
For those seeking additional ways to manage pudendal neuralgia, alternative therapies can offer valuable support alongside conventional treatments. These therapies focus on symptom relief and improving overall quality of life.
- Yoga and Pilates: Gentle exercises like yoga and Pilates can strengthen the pelvic floor muscles, enhance flexibility, and reduce pain. These practices also promote relaxation and stress reduction, which can help manage pudendal neuralgia symptoms. Specific poses and movements can be tailored to avoid putting pressure on the pelvic region.
- Mind-Body Therapies: Techniques such as meditation, deep breathing, and progressive muscle relaxation can help manage stress and anxiety, which are common in individuals with chronic pain. These therapies can also improve sleep quality, which is often disrupted in those suffering from pudendal neuralgia.
- Massage Therapy: While not a primary treatment for pudendal neuralgia, massage therapy can offer temporary relief by releasing tension and tightness in the surrounding muscle tissue. A licensed massage therapist can work with a healthcare provider to develop a personalized massage plan that addresses the individual’s specific needs.
- Chiropractic Care: Chiropractic adjustments may help realign the spine and pelvis, reducing pressure on the pudendal nerve and alleviating symptoms. It is crucial to find a chiropractor experienced in treating pudendal neuralgia and to discuss any concerns with a healthcare provider before starting treatment.
- Physical Therapy Modalities: Physical therapists may use modalities like heat, cold, or electrical stimulation to reduce pain and inflammation. These modalities can be used in conjunction with pelvic floor physical therapy to provide comprehensive care.
While alternative therapies should not replace traditional treatments, they can complement them effectively. Individuals with pudendal neuralgia should consult with their healthcare provider before starting any alternative therapies to ensure they are safe and appropriate for their specific condition.
Lifestyle Changes and Pain Management
Many patients with pudendal neuralgia find relief through lifestyle modifications that reduce pressure on the pudendal nerve. These may include:
- Avoiding activities that aggravate symptoms, such as prolonged sitting, biking, or heavy lifting.
- Using cushions designed to reduce pressure on the pelvic region.
- Incorporating gentle stretches and exercises to maintain pelvic mobility without straining the pelvic floor.
Frequently Asked Questions (FAQs)
1. Can men fully recover from pudendal neuralgia?
While recovery can take time, especially in cases of chronic pudendal neuralgia, many men experience significant improvement with a combination of pelvic floor physical therapy, nerve blocks, and lifestyle changes.
2. Is pudendal nerve decompression surgery necessary?
Decompression surgery is considered only when conservative treatments like physical therapy, nerve blocks, and medication fail to provide adequate relief.
3. How long do pudendal nerve blocks last?
A pudendal nerve block can provide relief ranging from a few hours to several months, depending on the severity of the nerve irritation.
4. What exercises should men avoid with pudendal neuralgia?
Men with pudendal neuralgia should avoid exercises that place excessive pressure on the pelvic floor, such as heavy lifting, squats, or prolonged cycling.
5. Can pelvic surgery cause pudendal neuralgia?
Yes, pelvic surgery can sometimes lead to pudendal nerve damage, resulting in pudendal neuralgia. It’s important to discuss risks with your surgeon before any procedure.
This condition can be managed in the right setting and with the right clinician. Savas Koutsantonis PT, DPT, CMTPT is a male physical therapist with an extensive history in treating persistent chronic pain conditions, especially concerning male pelvic health.
Click here to book your appointment with the One on One Physical PT staff
About The Author
 Dr. Savas Koutsantonis, PT, DPT, CMTPT
Dr. Savas Koutsantonis, PT, DPT, CMTPT
Male pelvic floor physical therapist with over 35 years of clinical experience specializing in chronic pain conditions, male pelvic health, headache, and jaw issues.