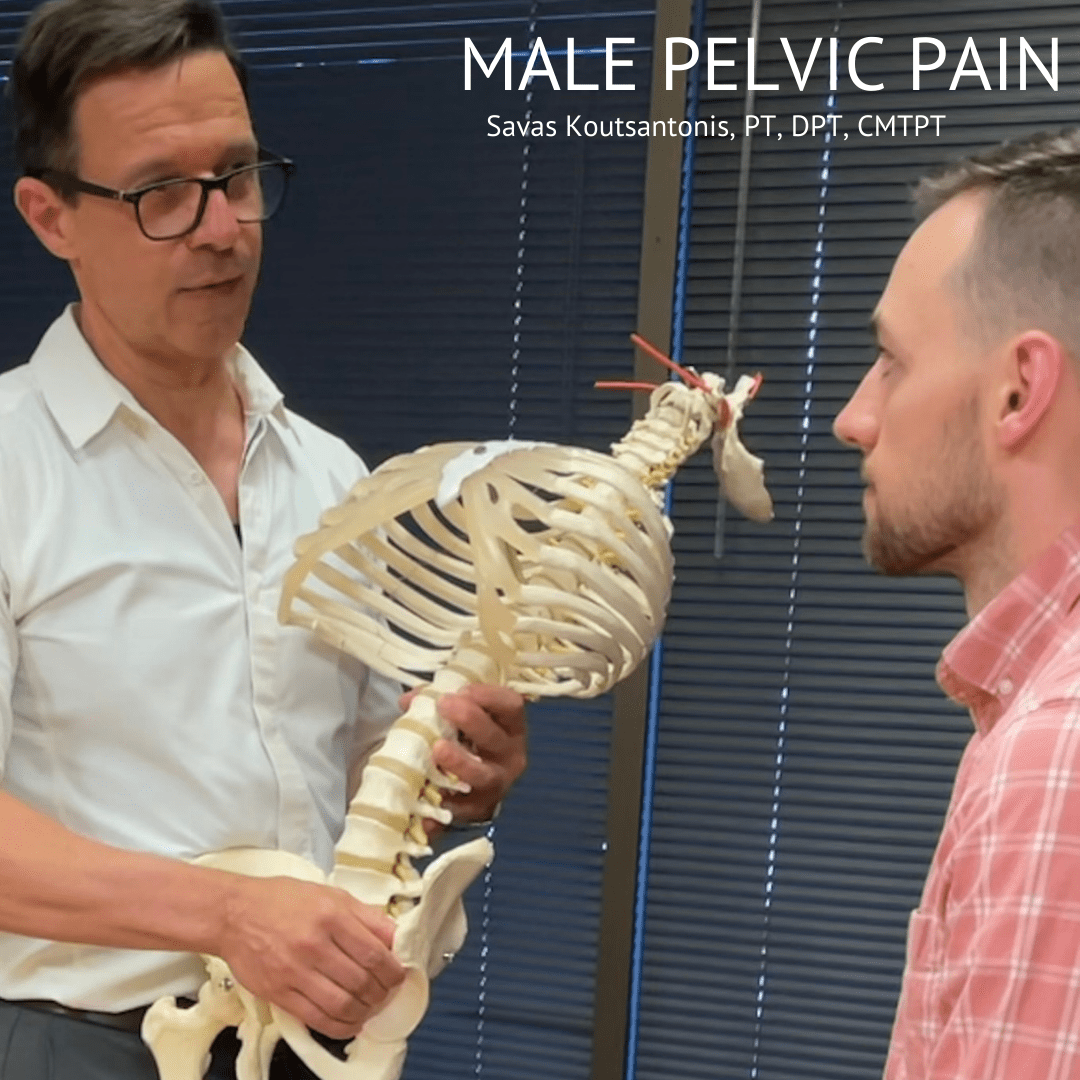
Male Pelvic Pain
…it’s more common than you think…and yes, it can be treated!
With June being Men’s Health Awareness Month, we wanted to bring awareness to a problem that is commonly misdiagnosed.
Men with pelvic pain are almost always misdiagnosed as “prostatitis” and are prescribed rounds of antibiotics even though they do not have an infection. More commonly referred to as Chronic Pelvic Pain Syndrome (CPPS) which can present as perineal (pelvic floor) and genital pain. The prevalence of CPPS in the United States ranges from 2-16% with a median age of 43. CPPS is underreported, rarely discussed but can drastically affect the quality of life. Symptoms of CPPS can vary from person to person. It can be constant or intermittent, sharp/intense versus dull/achy. Can present as pain, pressure, burning, or itching. Additional symptoms may include:
- Pain in the penis, scrotum/testicles, perineum, rectum, or tailbone
- Pain with urination
- Difficulty initiating urination
- Increased frequency of urination
- Pain during or after ejaculation
- Constipation and/or painful bowel movements
- diarrhea
- Bloating
- Erectile dysfunction and reduced ejaculation strength
Other Related Diagnoses can be Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome, Interstitial Cystitis.
Causes of Pelvic Pain:
- Post-surgical including vasectomy, prostatectomy, hernial repair
- Orthopedic issues including spine, hip, leg, pelvic
- Direct trauma
- Aggressive or excessive exercise with straining
- High-stress lifestyle with chronic “holding” patterns
- Excessive sitting including working at desk or biking
- Chronic constipation with abdominal straining
- Jelquing or genital enlargement exercises
- The high tone of the pelvic floor with poor functional coordination/control
What to do if you suspect you are having pelvic pain.
First thing is to consult a Physical Therapist that specifically works on male issues. Then they will review:
- A thorough review of history, symptoms, and lifestyle
- Thorough physical examination of tissues, muscles, joints, nerves for irritation, tone, and mobility
- Assessment of active patterns and coordination
- Use of rehabilitative ultrasound imaging to assess internal function and provide biofeedback
- Provide manual treatment including trigger point release, mobilization of joints and tissue
- Incorporate relaxation and breathing techniques, self-awareness of holding patterns
- Home self-management program instruction
- Therapist – patient open and accessible communication
Sometimes, it’s kind of nice to have a male physical therapist treating your male pelvic issues which can be a bit embarrassing or difficult to discuss.
Just remember you are not alone in this…
Other Blogs about Male Health
About The Author
 Savas Koutsantonis, PT, DPT, CMTPT brings over 30 years of physical therapy experience to One on One, and holds a Doctorate of Physical Therapy Degree from A.T. Still University of Health Sciences, Arizona School of Health Sciences. Within his scope of practice, Savas has advanced training in osteopathic manual therapy, Norwegian-based medical exercise technique, and is a Polestar trained Pilates instructor, which he uses along with RedCord apparatus to implement a comprehensive approach to back and orthopedic rehabilitation. He is certified to perform Trigger Point Dry Needling through Myopain Seminars. Savas is also an instructor for Myopain Seminars, teaching and certifying health care professionals around the country in Dry Needling.
Savas Koutsantonis, PT, DPT, CMTPT brings over 30 years of physical therapy experience to One on One, and holds a Doctorate of Physical Therapy Degree from A.T. Still University of Health Sciences, Arizona School of Health Sciences. Within his scope of practice, Savas has advanced training in osteopathic manual therapy, Norwegian-based medical exercise technique, and is a Polestar trained Pilates instructor, which he uses along with RedCord apparatus to implement a comprehensive approach to back and orthopedic rehabilitation. He is certified to perform Trigger Point Dry Needling through Myopain Seminars. Savas is also an instructor for Myopain Seminars, teaching and certifying health care professionals around the country in Dry Needling.