What is a frozen shoulder?
Frozen shoulder, or “adhesive capsulitis,” is a condition that involves a tightening of the capsule and ligaments around the shoulder. Inflammation within the shoulder joint and an increase in nerve growth around the shoulder complex results in pain, stiffness, and limited shoulder range of motion.1
It is estimated that 2-5.3% of the general population experiences frozen shoulder.1 Studies have shown that this pathology is more prevalent among females and individuals between 40 and 70 years old, with the peak incidence occurring between 51 and 55.1,2
There are four stages of frozen shoulder, each with distinct characteristics and time frames.1,2 Overall, frozen shoulder can last up to two years.
Inflammatory stage: characterized by sleep disturbances and sharp pain both at rest and at end range shoulder movement. This initial stage lasts roughly three months.
“Freezing” stage: characterized primarily by pain at night and progressive limitation in shoulder range motion. when lifting the arm above shoulder height, rotating the arm out to the side, and reaching behind the back. This stage lasts between months three and nine.
“Frozen” stage: characterized by pain and limited shoulder range of motion. This stage generally lasts between months nine and fifteen.
“Thawing” stage: characterized by a gradual decrease in shoulder pain and improvements in shoulder range of motion. This stage lasts between months fifteen and twenty-four.
What causes frozen shoulder?
The exact cause of frozen shoulder is unknown. However, there are a number of risk factors that contribute to the development of this condition. In addition to trauma, prolonged immobilization, and previous episodes of frozen shoulder in the opposite arm, research has identified the following risk factors: 1,2,3
Systemic factors: diabetes mellitus, thyroid dysfunctions, hypoadrenalism, Dupuytren’s disease
Intrinsic factors: rotator cuff pathologies, acromioclavicular arthritis, biceps tendinitis
Extrinsic factors: cardiopulmonary dysfunctions, cervical disc disease, stroke, Parkinson’s disease, and humeral. fractures
How is frozen shoulder treated?
There is a wide variety of conservative and surgical treatments for frozen shoulder. Corticosteroids, taken to decrease pain and moderate the inflammatory process, have been shown to improve both shoulder range of motion and overall function of individuals with this condition.1,3 Hydrodilatation, a process that involves injecting the shoulder with an anesthetic to expand and stretch the shoulder capsule, is a treatment method that has also been shown to improve overall function.3 Manipulation under anesthesia, a common surgical procedure for frozen shoulder, is a method designed to decrease adhesions around the shoulder capsule to improve range of motion. While all of these methods can lead to improved pain, range of motion, and function, combining each of these methods with physical therapy may lead to greater improvements.3
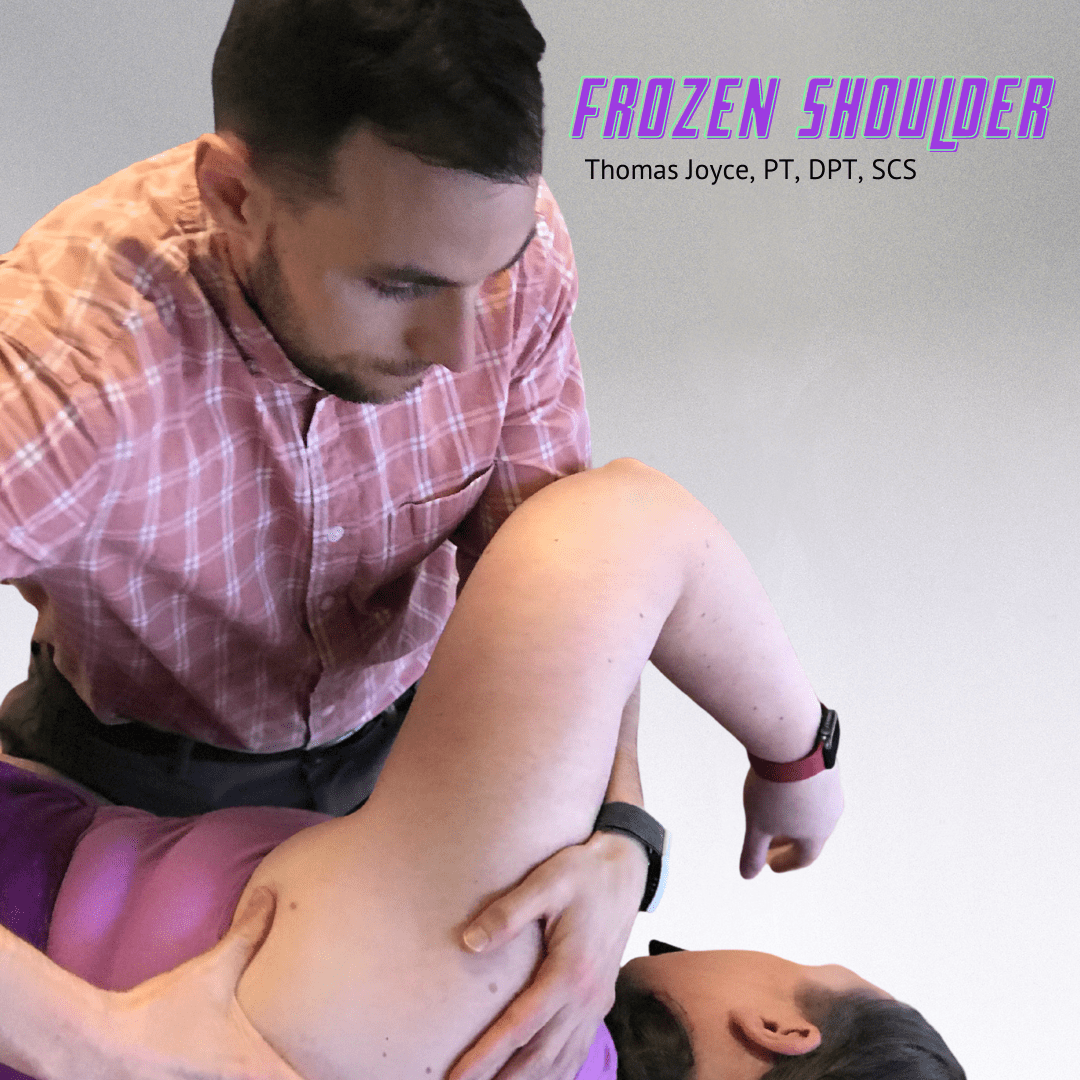
Physical therapy for frozen shoulder typically includes joint mobilization, guided stretching, and education regarding proper activity modification and exercise progression. Like other methods, these techniques lead to improvements in pain, range of motion, and function in individuals with this condition.1,2,3 Physical therapy will also incorporate strengthening exercises, but treatment methods that are often overlooked include breathing and neuromuscular control exercises designed to address muscular imbalances and promote proper movement patterns around the shoulder and thoracic spine. These treatment techniques enhance the shoulder’s ability to operate properly during daily and physical activity.
Treatment for frozen shoulder can vary from person to person. For an individualized treatment plan and best management of symptoms, contact One on One today!
About The Author
 Dr. Thomas (TJ) Joyce, PT, DPT, SCS joins One on One Physical Therapy after completing the Sports Physical Therapy Residency at The Ohio State University. While at OSU, his research focused on the influence of shoulder range of motion on the shoulder and elbow kinetics in baseball pitchers. Dr. TJ received his Doctor of Physical Therapy degree from Duke University. He has a passion for working with high school, recreational, collegiate, and professional athletes across many sports and enjoys working with athletes of all ages. Dr. TJ is a Georgia native who earned his Bachelor of Arts degree in philosophy and religious studies from Rhodes College in 2011. During his time at Rhodes, he ran track and played middle infield for the baseball team. He is a Certified Strength and Conditioning Specialist and a Certified Olympic Weightlifting Coach. When Dr. TJ is not working with his patients, he enjoys lifting weights, playing sports, and cheering on his Georgia Bulldogs.
Dr. Thomas (TJ) Joyce, PT, DPT, SCS joins One on One Physical Therapy after completing the Sports Physical Therapy Residency at The Ohio State University. While at OSU, his research focused on the influence of shoulder range of motion on the shoulder and elbow kinetics in baseball pitchers. Dr. TJ received his Doctor of Physical Therapy degree from Duke University. He has a passion for working with high school, recreational, collegiate, and professional athletes across many sports and enjoys working with athletes of all ages. Dr. TJ is a Georgia native who earned his Bachelor of Arts degree in philosophy and religious studies from Rhodes College in 2011. During his time at Rhodes, he ran track and played middle infield for the baseball team. He is a Certified Strength and Conditioning Specialist and a Certified Olympic Weightlifting Coach. When Dr. TJ is not working with his patients, he enjoys lifting weights, playing sports, and cheering on his Georgia Bulldogs.
References
- Martin KJ, et al. Shoulder pain and mobility deficits: adhesive capsulitis. Kelley MJ, Shaffer MA, Kuhn JE, Michener LA, Seitz AL, Uhl TL, Godges JJ, McClure PW. J Orthop Sports Phys Ther. 2013 May;43(5):A1-31.
- Nakandala P, Nanayakkara I, Wadugodapitiya S, Gawarammana I. The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: A systematic review. J Back Musculoskelet Rehabil. 2020 Nov 6. doi: 10.3233/BMR-200186. Epub ahead of print. PMID: 33185587.
- Ramirez J. Adhesive Capsulitis: Diagnosis and Management. Am Fam Physician. 2019 Mar 1;99(5):297-300. PMID: 30811157.